Introduction
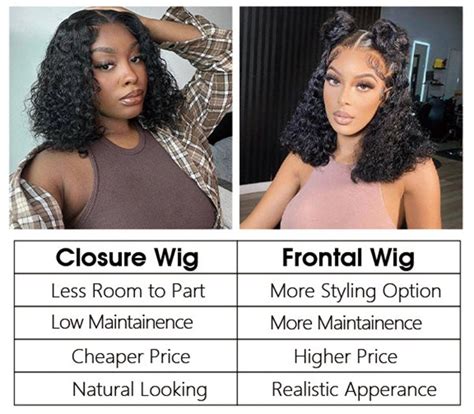
Maxillofacial prostheses play a pivotal role in restoring the function and aesthetics of patients who have undergone facial surgery or trauma. Prostheses can be classified into two primary types: closure and frontal. Understanding the differences between these two types is crucial for practitioners and patients alike.

Closure Prostheses
Closure prostheses, also known as obturators or defects, are designed to fill surgical defects within the oral cavity or nasal passages. They serve several critical functions:
- Restoring function: Closure prostheses enable patients to speak, swallow, and breathe effectively by obstructing gaps that may impair these functions.
- Preventing infection: By sealing defects, closure prostheses prevent food and fluids from entering the surgical site, reducing the risk of infection.
- Supporting tissue: They provide support to surrounding tissues, preventing tissue collapse and promoting healing.
Types of Closure Prostheses:
Closure prostheses are customized to fit the unique defects of each patient. Common types include:
- Obturator prostheses: Designed to fill defects in the palate or maxilla, allowing for normal swallowing and speech.
- Nasal prostheses: Replace missing tissue in the nasal cavity, preventing nasal discharge and improving airflow.
- Orbital prostheses: Used to fill orbital defects, restoring the contour of the face and allowing for eye movement.
Frontal Prostheses
Frontal prostheses, also known as facial prostheses, are used to reconstruct the external facial appearance. They are indicated primarily for patients who have lost significant facial tissue due to trauma or surgery.
- Restoring aesthetics: Frontal prostheses aim to recreate the aesthetic contours of the face, improving the patient’s self-esteem and social well-being.
- Relieving discomfort: They can provide coverage and cushioning for sensitive areas, reducing pain and discomfort caused by exposed tissue.
- Protecting tissues: Frontal prostheses shield vulnerable tissues from environmental factors such as cold, wind, and UV radiation.
Types of Frontal Prostheses:
Frontal prostheses are tailored to meet individual patient needs. Common types include:
- Nasal prostheses: Replace missing nasal tissue, restoring the shape and functionality of the nose.
- Ear prostheses: Reconstruct lost ear tissue, providing a natural and lifelike appearance.
- Orbital prostheses: Used to replace an entire eye socket and match the appearance of the contralateral eye.
- Chin prostheses: Enhance the contour of the chin, creating a more balanced facial profile.
Materials Used
Both closure and frontal prostheses are typically made from a combination of materials, including:
- Silicone: Provides durability, flexibility, and color stability.
- Acrylic: Offers strength, rigidity, and ease of fabrication.
- Medpor: A porous polyethylene material used for structural support and tissue integration.
- Biomaterials: Advanced materials that promote tissue healing and integration.
Fabrication Process
The fabrication process for both closure and frontal prostheses involves the following steps:
- Impression taking: A mold of the surgical defect is created using dental impression materials.
- Model creation: A model of the defect is constructed based on the impression.
- Design: The prosthesis is designed using software and sculpting techniques.
- Fabrication: The prosthesis is created using materials such as silicone or acrylic.
- Coloring: The prosthesis is colored to match the surrounding skin tone or tissue.
Clinical Considerations
When selecting between closure and frontal prostheses, practitioners must consider several clinical factors:
- Defect size and location: The size and location of the defect will determine the type and complexity of the prosthesis required.
- Patient’s needs and desires: The patient’s individual needs and aesthetic preferences should be taken into account.
- Surgeon’s experience and skills: The surgeon’s experience and skills in maxillofacial prosthetics will influence the outcome of the procedure.
Future Directions
Advancements in materials and technology are constantly driving the development of new and innovative maxillofacial prostheses.
- Personalized prostheses: 3D printing techniques enable the creation of highly customized prostheses that precisely match the patient’s anatomical features.
- Tissue engineering: Researchers are exploring the use of tissue engineering to generate new tissue that can be used to repair defects and improve the integration of prostheses.
- Biomimetics: By mimicking natural tissues, biomimetic materials can offer improved function, durability, and aesthetic outcomes.
Conclusion
Closure and frontal prostheses play a vital role in restoring the function and appearance of patients who have undergone facial surgery or trauma. Understanding the differences between these two types of prostheses is essential for optimal patient outcomes. As technology continues to advance, maxillofacial prostheses will continue to evolve, offering improved quality of life for patients and transformative possibilities in the field of facial reconstruction.